Progressive Myoclonic Epilepsies
What are progressive myoclonic epilepsies, known as PME?
Progressive myoclonic epilepsies (PME) are a group of more than 10 rare types of epilepsies that are “progressive.” People with PME have a decline in motor skills, balance and cognitive function over time.
People with one of the PMEs have a mix of myoclonic (rapid muscle jerks of various body parts) and tonic-clonic seizures. Other symptoms that usually happen later on are unsteadiness, muscle rigidity (tightness of the muscles), balance problems, and mental decline.
People with PME eventually need a wheelchair and significant help for normal daily activities. They also have a shortened life span.
Who gets it and when?
PME is a group of rare disorders that are genetic. PME occurs worldwide, but exact rates for most subtypes are unknown.
- One of the most common forms, Lafora disease, occurs in about 1 in 20,000 births in Finland.
- Other regions where some forms of PME are more common generally include areas with more interfamilial (belonging to the same family) marriages.
Usually, there is no family history of the disease. Most forms of PME are inherited in an autosomal recessive pattern. This means there is an abnormal gene from both parents.
- For example, when first cousins have children together, there is a higher risk of passing down two copies of the abnormal gene carried within the same family.
- PME can also occur in children of non-related parents. These forms are among the rarest subtypes of PME.
Progressive myoclonic epilepsies affecs both sexes equally. The age of onset can vary from infancy to adulthood, depending on the specific type of myoclonic epilepsy and the underlying genetic mutation.
- The most common forms are first noted in early adolescence to late childhood. They happen in otherwise normal and previously healthy children.
- Because the inheritance pattern and disease course can vary significantly based on the genetic cause, diagnosing the gene is important for counseling the patient and the family.
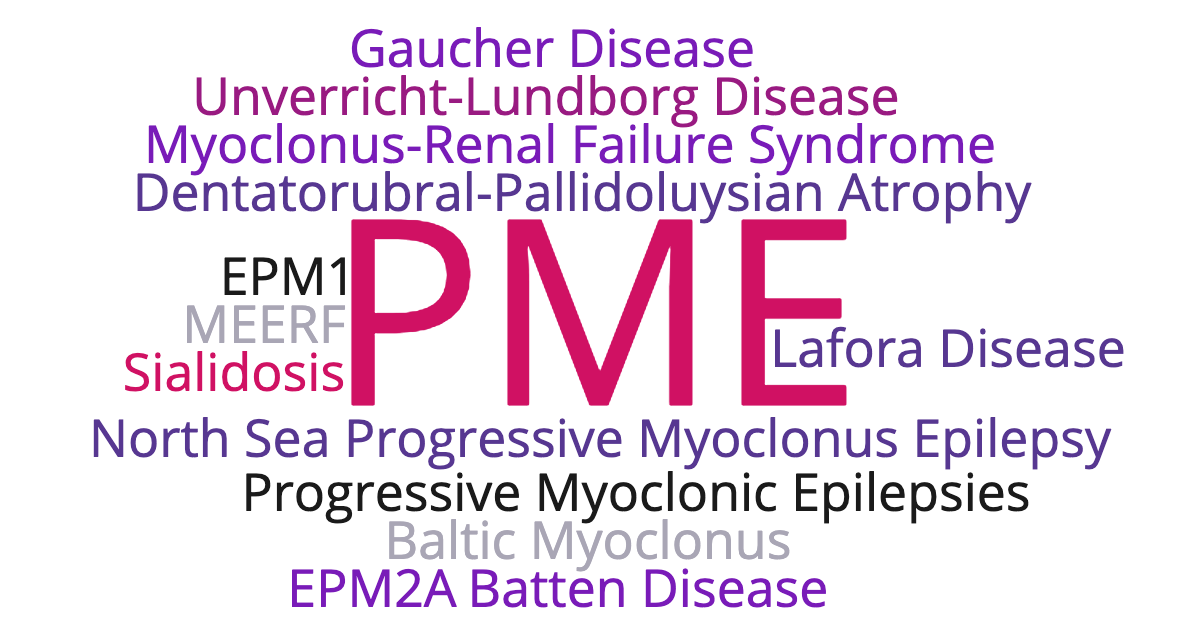
What are the types of PME and how are they different?
PME is a group of epilepsy syndromes with various names. The most common forms of PME are described below.
For all types of PME, the age of onset varies and usually occurs between 6-16 years of age. They all have difficult to treat seizures, balance and coordination problems, and cognitive decline over time.
Unverricht-Lundborg Disease
- This type of PME is also called Baltic myoclonus and epilepsy, progressive myoclonus 1, and EPM1.
- This is the most common form of PME worldwide.
- It is caused by a mutation within a protein that is important for the proper function of the lysosome (the part of a cell that breaks down waste). There are over 14 different known genetic mutations.
- A distinguishing feature (in addition to those above) is dysarthria (trouble with speaking clearly), dysphagia (difficulty swallowing/eating), and tremor.
- An earlier onset of symptoms predicts a more severe course.
- Although life expectancy is shortened, it is extremely variable. In the past, life expectancy was 8 - 15 years after symptoms began. Yet with newer supportive treatments, some people with milder forms of EMP1 can live into their 70s.
Lafora Disease
- This type of PME is also called Lafora epilepsy, progressive myoclonus 2, and EPM2A.
- Lafora disease is characterized by the buildup of Lafora bodies (carbohydrate/surger particles) in cells in the brain and spinal cord. The Lafora bodies can also be found in muscles or skin cells.
- Although this syndrome begins more specifically in adolescents (12-15 years), there is a form of Lafora disease that can start as young as age 5.
- After seizures start, there is a rapid worsening of cognition (thinking), visual loss, and coordination. This differs from EPM1, which has a significant motor decline first.
- Cognitive decline impairs motor planning, causing difficulty with brushing teeth, brushing hair, and bringing utensils to the mouth. The decline usually occurs within the first 10 years. People with Lafora disease also have a shortened life span.
Neuronal Ceroid Lipofuscinoses
- This type of PME is more commonly called Batten disease.
- Batten disease refers to a family of about seven disorders within the neuronal ceroid lipofuscinoses group.
- These diseases are caused by an error in a lysosomal enzyme needed to help breakdown and get rid of unneeded material within a cell. Without the enzyme, material builds up in cells of the nervous system, causing them to malfunction.
- It can begin at different ages, including in infants, adolescents and adults.
- The first symptoms are myoclonus and generalized tonic-clonic seizures. These are followed by cognitive and emotional decline, motor decline, and visual loss leading to blindness (from damage to the retina).
- The length of survival depends on the specific subtype, but all of these lead to early death.
Other Less Common Forms of PME
Less common forms of PME include
- Mitochondrial encephalopathies
- Other disease of metabolism:
- Sialidosis
- Myoclonus Epilepsy and Ragged-Red Fibers (MERRF)
- Type 3 Neuronopathic Gaucher Disease
- Dentatorubral-Pallidoluysian Atrophy
- Myoclonus-renal Failure Syndrome
- Progressive Myoclonus Epilepsy-Ataxia Syndrome
- North Sea Progressive Myoclonus Epilepsy
- Myoclonus Epilepsy and Ataxia due to pathogenic variants in the potassium channel
What type of seizures and other associated symptoms are seen?
The most common type of seizures are myoclonic and generalized tonic-clonic seizures.
- Myoclonic seizures are often triggered by a stimulus, like lights flashing, being startled, having stressful thoughts or emotions, or rapid movements/actions. They may initially be hard to distinguish from myoclonic seizures seen in other epilepsy syndromes, such as juvenile myoclonic epilepsy (JME). Compared to JME, they do not respond well to medications and get worse over time.
- Generalized tonic-clonic seizures are also common in PME.
- Focal seizures are also seen and often have visual symptoms, including visual hallucinations, with EEG (electroencephalogram) discharges from the visual regions of the brain.
- Tonic seizures can also occur (whole body may become stiff).
- Lastly, absence seizures, noted by staring episodes that cannot be interrupted, can also be part of PME.
Other features of the disease include
- Problems with memory and thinking that worsens over time.
- Some forms of PME have a more drastic motor decline. This includes a worsening ataxia (decrease in balance and coordination), apraxia (decline in motor planning and coordination), and sometimes slowness and stiffness of movements.
- The apraxia can be a significant challenge. People lose the ability to walk because their brain can no longer process how to coordinate the movements of placing one foot in front of the other. Other tasks, such as bringing utensils to the mouth and brushing hair and teeth, become difficult. Overtime, most people need a wheelchair and 24-hour help.
How is it diagnosed?
Diagnosing the different types of PME can be difficult.
- The early way to tell the difference is an EEG with background slowing.
- Symptoms like stimulus induced myoclonic jerks, cognitive decline and motor slowing, generalized tonic-clonic seizures, or visual/occipital seizures help narrow the diagnosis.
- Most importantly, the presence of slowing on the EEG should raise suspicion for PME and, if present, lead to further testing, including genetic and enzyme testing.
- A skin biopsy may be done.
- Genetic testing is becoming more easily available and is currently the most definitive way to diagnosis PME.
How is PME treated?
The medical treatment of progressive myoclonic epilepsy is limited to supportive and symptomatic treatment.
The treatment is often successful only for a few months or years. There is no current cure for PME.
People with PME require many seizure medications, comprehensive rehabilitation treatment, and treatment of mood symptoms. Social and psychological support are also among the most important forms of treatment for the person with PME and their family.
Most people require more than one seizure medication as the disorder progresses. With time, the medications become less effective while side effects become more severe. In such cases, it is often worthwhile to try lower doses.
- Valproate (Depakote) is most commonly used.
- Other seizure medicines used include levetiracetam (Keppra), topiramate (Topamax), clonazepam (Klonopin), and zonisamide (Zonegran). Clobazam (Onfi) and brivaracetam (Briviact) may also have benefit.
- While lamotrigine (Lamictal) can be used, in rare patients the drug can make seizures worse and, thus, generally should be avoided.
- Medications to be avoided, as they can make myoclonic jerks and balance worse, include phenytoin (Dilantin), carbamazepine (Tegretol), oxcarbazepine (Trileptal and Oxtellar XR) and eslicarbazepine (Aptiom), as well as GABAergic drugs including tiagabine (Gabitril) and vigabatrin (Sabril). Gabapentin (Neurontin) and pregabalin (Lyrica) may aggravate myoclonus.
- In mitochondrial forms of PME, valproic acid should be avoided.
- Research trials with new molecules are another option for treatment for some of the PMEs. In the future, genetic therapies may be possible.
What's the outlook?
The outlook is generally unfavorable. Seizures are difficult to control and people often lose abilities involving thinking and movement. However, the outlook for different types of PME can vary from person to another.
After diagnosis, genetic counseling can help provide information to families about how the PME may progress, including
- Timeframe of decline
- Treatments
- Risk of disease in genetically related members of the family
There are support groups for people with PME and families that can provide information, support, shared experiences and connection.
Research is ongoing with the goal of identifying ways to correct the disruption of the faulty gene.
Resources
- International League Against Epilepsy (ILAE) on progressive myoclonus epilepsy
- National Organization for Rare Disorders (NORD) on PME
- Learn about the Rare Epilepsy Network (REN)
- What’s a clinical trial and why should you join one? Find out here.
- Find a Clinical Trial
- Information on current clinical trials also can be found at www.clinicaltrials.gov.
- Find epilepsy therapies in various stages of development in our Epilepsy Pipeline Tracker.
Resources
Epilepsy Centers
Epilepsy centers provide you with a team of specialists to help you diagnose your epilepsy and explore treatment options.
Epilepsy Medication
Find in-depth information on anti-seizure medications so you know what to ask your doctor.
Epilepsy and Seizures 24/7 Helpline
Call our Epilepsy and Seizures 24/7 Helpline and talk with an epilepsy information specialist or submit a question online.
Tools & Resources
Get information, tips, and more to help you manage your epilepsy.


